What The Heck Is A Pelvic Floor & How To Take Care Of Yours.
Hello!
There are some words regarding genital anatomy in this blog that might make you a bit uncomfortable, so let’s get them out of the way. Vagina, vulva, clitoris, anus, penis, scrotum and prostate. Unless you’re a toddler with a limited vocabulary or participating in intimate play, hopefully, the journey of your genital vernacular has evolved. Let’s stop referring to the vagina as down there, vajaja and pussy, and the penis as pee-pee, dick or Peter.
What is the Pelvic Floor?
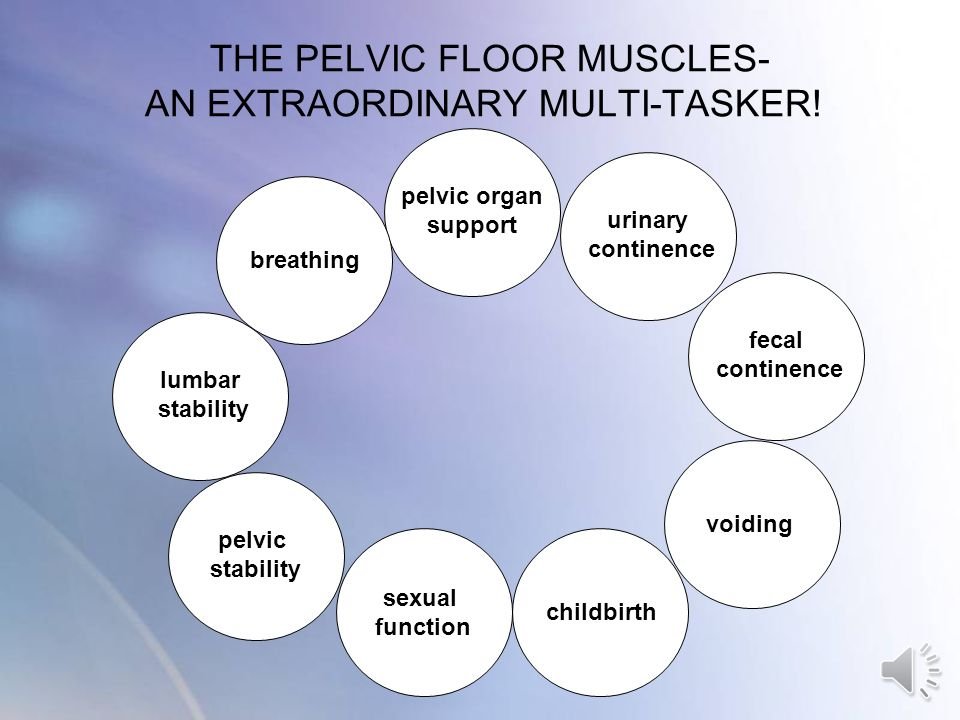
The pelvic floor is a group of muscles and ligaments located at the base of the pelvis. These muscles stretch from the pubic bone at the front to the tailbone at the back and from side to side, forming a hammock-like structure. They support the pelvic organs, including the bladder, uterus (in women), bowel, and prostate in men.
When the pelvic floor muscles and ligaments are not functioning well, mild to severe symptoms can occur that could greatly impact one's quality of life.
I’ve heard about the pelvic floor, but I’ve never paid much attention until I was recently forced to. I’ve dealt with recurrent urinary tract infections (UTIs) since 2009, and they have become severe since January, with me taking more than five rounds of antibiotics. With the help of a bladder ultrasound and diagnosis and treatment from a pelvic floor physiotherapist, I’ve learned that my pelvic floor is not functioning correctly because of a combination of tight and weak muscles and mild prolapse of the uterus and bladder. This explains so much, and I’ll provide more details about my treatments below.
I’ve also discovered that so many individuals, more women than men, are struggling with pelvic floor discomfort, and I’m grateful that more treatment options are now available.
Pelvic Floor Gender Differences
Pelvic Floor Functions
Pelvic Floor Dysfunction
When your pelvic floor muscles and organs are not functioning correctly, you may experience a plethora of symptoms:
1. Urinary issues:
Difficulty urinating or frequent urges to urinate.
Painful urination.
Stopping and starting while urinating.
Urinary incontinence (leakage).
The bladder does not completely empty after urination.
Frequent urinary tract infections (UTIs).
2. Bowel problems:
Constipation or straining during bowel movements.
The feeling of incomplete bowel movements.
Fecal incontinence.
3. Pain and discomfort:
Lower back pain.
Pain in the pelvic region, genitals, or rectum.
Pressure or heaviness in the pelvic area.
4. Sexual dysfunction:
Pain during sexual intercourse (for women.)
Erectile dysfunction (for men).
5. Other:
Uterine prolapse-this is a form of pelvic organ prolapse in which the uterus and a portion of the upper vagina protrude into the vagina canal.
If you’ve had surgery in the pelvic floor area, it may have contributed to its dysfunction.
There are many possible causes of pelvic floor dysfunction: childbirth, pelvic muscles weakening because of aging and hormonal changes, persistent coughing, chronic straining, and weight gain,
Treatment
There was a time when the only treatment option was to perform hundreds of Kegel exercises daily to strengthen the pelvic floor. Kegel exercises involve contracting your pelvic floor muscles. Stopping the flow of urination is considered a Kegal contraction.
Kegels are not enough. You must also ensure a strong core, including your abdominals, glutes, diaphragm, and back muscles. Seeing a pelvic floor physiotherapist is a must to make a diagnosis and develop a treatment plan.
My Story
My daughter was born in 1990, and shortly after her birth, I started to experience mild urinary incontinence. Each year, the incontinence became worse to the point where I could barely move without wetting myself.
In 2008, I had surgery where a tape was placed across my urethra to support it. It was successful, and I never had urinary incontinence again. Then in 2009, I started to experience urinary tract infections. At first, it was 1-2 per year, and with each year, the numbers increased, and in the last few years, I’d have about 6 per year. Many years ago, I saw the surgeon who performed the surgery, and after an examination, she didn’t see any issues and prescribed 3 months’ worth of antibiotics. This helped for a few months, and then they started again.
I was diagnosed with Lyme Disease in November 2022, and since then, the frequency of my infections has doubled, and there is no doubt that Lyme has contributed to the increase.
My family doctor sent me for a bladder ultrasound about 8 months ago, and it showed that my bladder and urethra still contained urine after urination. He feels strongly that the 2009 procedure is the major cause of my chronic UTIs. He suggested that I see a pelvic floor physiotherapist.
I started seeing a pelvic floor physiotherapist in May. She took my history, performed an internal examination, and informed me that my pelvic floor was a mess. She has given me numerous exercises that require me to simultaneously contract my pelvic floor and core muscles while performing them. These exercises are not easy, and you must consistently practice them at least three times a week and daily in the beginning.
Squating Position for Elimination
Elevating your knees above your pelvis and leaning forward makes it easier to completely empty your bladder and bowels.
She has taught me how to urinate properly. Yes, you read that correctly. She informed me how important it is to go when you feel the urge and to take a few minutes because you will probably void more than once. How often do we hold the urge and then rush the whole urination process?
I also purchased a step like the one in the above picture. I’m working with my naturopath and have made some dietary changes. I have been taking numerous supplements to replenish my gut with good bacteria and to support my bladder.
My family doctor is mindful of changing the antibiotics he prescribes to prevent antibiotic resistance. He has given repeats on all prescriptions, so I can easily access antibiotics in case I need them.
This multidisciplinary approach has not cured my chronic UTIs, but for the first time in a long time-15 years, I feel like I’m on the path to recovery. Knowing their cause has been so helpful because I was starting to lose it.
What to do if you have pelvic floor dysfunction symptoms?
Don’t wait. See your family doctor, and if you don’t have one, go to a walk-in clinic or emergency department. Depending on your symptoms, push for a bladder/pelvic ultrasound to see if any anatomical issues are the cause of your symptoms. See a pelvic floor physiotherapist for a thorough assessment and treatment plan. They are highly trained in this area, and I feel that they are the most equipped. If you are dealing with any indication of prolapse of any of your pelvic floor organs, seek immediate help. Things will only worsen if you wait.
I’m grateful for the excellent health practitioners I work with and feel confident I’m progressing towards recovery. I did seek out help over the last 15 years, but I think I became complacent in my predicament when I should have been more insistent on finding the cause and a solution. Better late than never.
I hope you have never had to deal with any pelvic floor challenges, and if you have, I’d love to hear about what helped you.
Stay well.
Anita
Sources:
DISCLAIMER; The information provided on County Yoga Loft’s website blog is for general health care informational purposes only. All information on the site is provided in good faith. However, it should not replace consultation or advice from a physician and other healthcare practitioners. The use or reliance of any information contained on this site is solely at your own risk.